
-
Enquiry | Appointment
022-66776677 | +91-8779678354 -
Surgery | Bookings
+91-7208286076 | 022-66776677 -
Email
contact@envisioneyehospital.in
Cornea or Keratoconus Treatment
Cornea is the first coat of eye which is transparent circular structure. Functionally it acts as a lens responsible for focusing rays inside the eye. It is an important optical structure through which rays of light enter the eye. Any damage or injury to this delicate structure can lead to permanent loss of corneal transparency or in other words cause clouding and opacification.
Loss of corneal transparency prevents the entry of light rays into the eye and reduces vision. In cases of severe of damage, this can cause total loss of vision making the person visually handicapped. There are other conditions also such as malnutrition, Vitamin A deficiency, infection, certain corneal diseases such as ‘keratoconus’ and ‘corneal degeneration’, which can cause corneal blindness.
Corneal disease is third largest cause of blindness or low vision in Indian population. Corneal disorders encompass a wide spectrum of diseases most common of these are pterygium, Keratoconus, corneal dystrophy, corneal tears, corneal oedema , infective keratitis, contact lens related keratitis, allergic keratoconjunctivitis, each of these diseases need methodical approach and specialized care.
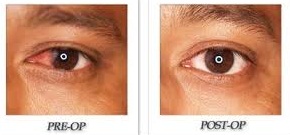
Pterygium
Pterygium is a veil like lesion that usually occurs in exposed part of white of the eye. This grows slowly over the cornea (the central black portion) and can obstruct vision or deteriorate vision by inducing cylindrical power
Symptoms of pterygium may include:
- Burning
- Itching
- Blurred vision
- Gritty feeling
- Sensation of a foreign body in the eye
Causes of Pterygium : significant risk factors include:
- Prolonged exposure to ultraviolet light
- Irritants such as dust and wind
- Dry eye
Treatment of Pterygium
Pterygium is not only cosmetically disfiguring but can affect the vision also. In view of this it is advisable to surgically excise it at the earliest. Surgical excision of pterygium is a simple day care procedure with no adverse effects.
Latest surgery method involves removing the pterygium tissue and placing a healthy tissue on bare area which prevents recurrence and is cosmetically very rewarding.
Surgery for pterygium is minimally invasive, sutureless and is very safe.
Pterygium does not respond to medical treatment of any kind be it in form of eye drops or ointment and surgical excision is the treatment of choice
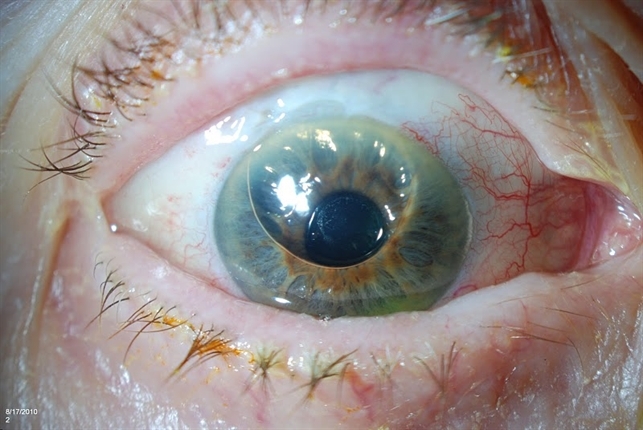
Symptoms & signs of Keratoconus
- Keratoconus causes myopia or nearsightedness & astigmatism.
- Frequent change in glasses prescription with fluctuation in vision.
- Glare & sensitivity to light especially during night.
- In advanced stage of Keratoconus corrective prescription glasses do not help patient to see clearly & they have to switch to using hard or semi-soft contact lenses.
- Keratoconus can be diagnosed at an early stage with detailed eye examination which includes Retinoscopy,
- Slit lamp examination & sophisticated tests like Topography to check the shape & curvature of cornea & Pachymetry to determine the thickness of the cornea.

Causes
Exact causes of Keratoconus is not known but latest research suggests that the cornea becomes weakened due to an imbalance of enzymes within the corneal tissue. Young patients produce high levels of free radicals which cause oxidative damage to the cornea in absence of protective enzymes causing thinning & bulging of the cornea.
Keratoconus also shows some genetic predisposition. It may transmit from parent to children & affect more than one family member. It is also associated with excessive rubbing as it is more common in allergic conjunctivitis patients who have itching & tend to rub their eyes more frequently.
Other risk factors are overexposure to ultra violet rays, chronic eye irritation & improperly fitting contact lenses.
Treatment Options
In early stages, when the cornea is still regular, corrective prescription glasses or soft contact lenses can help the patient. As keratoconus advances, the corneal surface becomes increasingly irregular & these options do not help adequately. In intermediate & advanced stage, various other treatment options & different types of contact lenses are available.
Rigid Gas permeable contact lenses : provide a smooth refractive surface replacing the irregular cone like surface of the cornea, thus enabling the patient to see clearly. Lens fitting in Keratoconus can be demanding & time consuming process. RGP lenses are not as comfortable as soft contact lenses.
Piggybacking Contact Lenses : a soft contact lens is first placed on cornea to give it a cushion like effect & RGP lens is fitted over it. Best features of both lenses are combined – makes the wearer comfortable & at the same time gives crisp & clear vision. The fitting should be perfect to ensure good oxygen permeability to the cornea as the patient will be wearing two lenses. However, with newer high oxygen permeable lenses this is not a problem.
Hybrid Contact lenses : uniquely designed wherein the central visual portion is made up of high oxygen permeable rigid material & peripheral anchoring portion is of soft hydrogel material. Maximizes the best features of both lenses & improves wearers comfort as well as visual performance in keratoconic eyes.
New Vistas In Surgical Treatment Of Keratoconous :Intacs (Intra Corneal Ring Segments)
Patients with moderate non progressive keratoconus who are intolerant to contact lenses are good candidates for INTACS . Use of INTACS not only improves the visual outcome it also reduces the dependency of patient on glasses or contact lenses. INTACS are rings made of inert material that are implanted in mid periphery of cornea . These rings significantly flatten the curvature of keratoconic cornea thus improving vision.
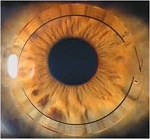
Benefits
- Simple 10 minute outpatient procedure
- Marked improvement in vision
- Removable & exchangeable
- Minimally invasive as compared to corneal transplantation
- Delays the progression of keratoconus
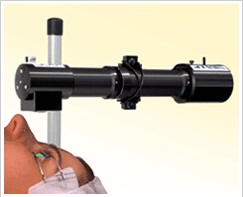
C3 – R (CORNEAL COLLAGEN CROSSLINKING)
Corneal collagen crosslinking with riboflavin is the latest addition to treatment options for early progressive keratoconus. This is minimally invasive day care procedure that stabilizes the keratoconus and prevents further deterioration of vision. With newer corneal topography equipments it is easy to pick up early keratoconus and C3R in such cases further progression of keratoconus and thus reduces visual morbidity. C3R is a safe procedure for early progressive keratoconus.
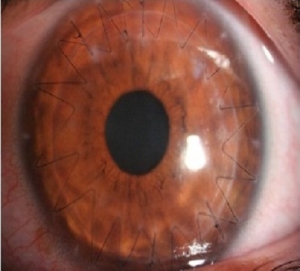
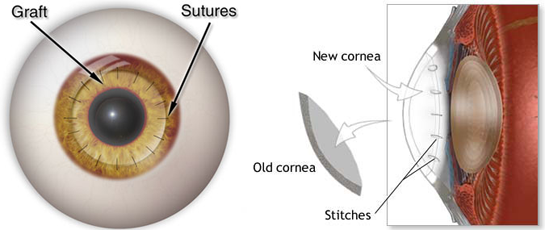
Penetrating Keratoplasty
This involves full thickness corneal transplantation, where the entire recipient cornea is replaced with full thickness donor cornea. This type of penetrating surgery is usually indicated for full thickness corneal opacity, failed grafts and macular corneal dystrophy. This type of surgery gives very good visual outcome but have along recovery period
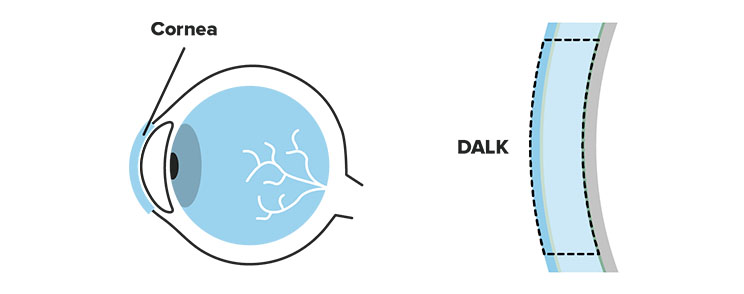
DALK (Deep anterior lamellar Keratoplasty)
This is one of the recent modification of keratoplasty where full thickness transplantation is not done. This type of transplantation involves replacing only the superior three diseased layers of cornea with healthy donor tissue .This procedure has faster recovery period and minimal risk of rejection. Also visual outcome is better. This surgery is indicated in cases with advanced Keratoconus, superficial scar.
Keratoplasty (Corneal Transplantation)
What is ‘Corneal Transplantation’?
Corneal transplantation / keratoplasty/ corneal grafting is the surgical procedure that restores sight in patients suffering from corneal blindness. In this surgical procedure, the diseased opaque cornea is replaced by a clear healthy donor corneal tissue which restores sight by allowing the light rays to enter the eye through transplanted clear cornea. This procedure of corneal grafting is possible only on the availability of donor cornea by process of eye donation. By donating eyes after death a human being can restore sight to a blind person. This gift of sight is invaluable for these visually handicapped persons.
Who can donate eyes?
Eye donation is possible only after death. Any person of any age, sex, caste or religion, people who wear glasses or have undergone an eye surgery can donate. People of any age group can pledge to donate his/ her eyes after death. Even if one has not pledged their eyes themselves, the relatives can give their consent for the donation of the eyes of the deceased.
Eye tissue procurement is performed within six hours of death. Families may proceed
with funeral arrangements without delay or interruption.
Great care is taken to preserve the donor’s appearance. The donor’s body is treated with respect at all times. Funeral arrangements, including a viewing, if desired, may proceed as scheduled.
Precautions after pledging eyes of deceased:
Switch off fans and switch on Air conditioner (if available). Raise the head of the deceased slightly by placing a pillow underneath. Place wet clean cloth over the closed eye lids. Please ensure that the eyelids are properly closed. Keep a copy of the death certificate ready (if available). Contact the nearest eye bank as quickly as possible.Give the correct address with specific landmarks or famous name of our area and mobile and residence number to enable the team of eye bank for locating the house easily.Give alternate cell number of any available relatives also.The eye bank team, which would have a trained technician and/or a registered medical practitioner, would remove the eyes after taking consent on a printed form in the presence of two witnesses and also take A small quantity of blood sample will be drawn to rule out communicable diseases.
Different Techniques of Keratoplasty Penetrating keratoplasty (Corneal Transplantation):
This is one of the recent modification of keratoplasty where full thickness transplantation is not done. This type of transplantation involves replacing only the superior three diseased layers of cornea with healthy donor tissue . This procedure has faster recovery period and minimal risk of rejection. Also visual outcome is better. This surgery is indicated in cases with advanced Keratoconus, superficial scar.
DALK (Deep anterior lamellar Keratoplasty)
This is one of the recent modification of keratoplasty where full thickness transplantation is not done. This type of transplantation involves replacing only the superior three diseased layers of cornea with healthy donor tissue . This procedure has faster recovery period and minimal risk of rejection. Also visual outcome is better. This surgery is indicated in cases with advanced Keratoconus, superficial scar.
DSEK (Descemets stripping endothelial keratoplasty)
DSEK is the most recent addition to the armamentarium to treat endothelial disease of cornea. This modification in keratoplasty replaces the diseased descemets and endothelium with healthy donor endothelium , descemets’ membrane and posterior stroma and requires no sutures. As this procedure is sutureless it has several advantages like faster recovery, better visual outcome and less risk of suture infection.
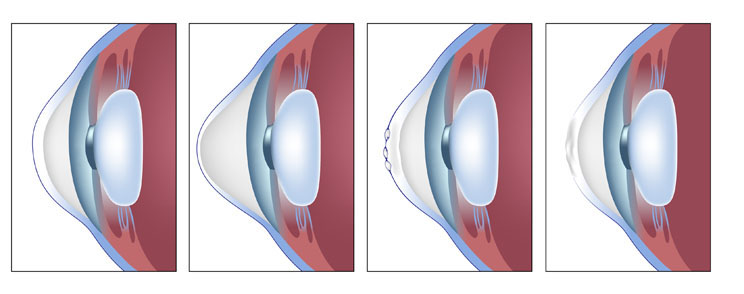
Descemet’s Membrane Endothelial Keratoplasty (DMEK)
Descemet membrane endothelial keratoplasty (DMEK) is the most recent solution to treat the decreased vision due to corneal oedema seen in Fuchs dystrophy, bullous keratopathy, and other causes of poor corneal endothelial function. There are three generations in the evolution of corneal transplantation and DMEK is the third and latest.
In DMEK the diseased innermost layer of the cornea is removed surgically and the corresponding thin layer from a healthy donor cornea is put in its place. The thin delicate transplant is secured with only an air bubble. The surgery can be combined with cataract surgery for patients who require both.
DMEK provides quick improvement in vision with reduced risk of rejection making it keratoplasty of choice in patients with corneal oedema.
Benefits
- 2.8 mm or smaller corneal incision
- No increase in corneal thickness
- Quick visual recovery so patients can resume daily activities early
- Better visual outcomes compared to other keratoplasty methods
- Reduced risk of vision threatening graft rejection episodes
